Daniel Giannetti

A cure for diabetes?
In a truly exciting advancement in the treatment of type 2 diabetes, Chinese researchers have successfully demonstrated the use of transplanted stem cell-derived islet tissue for a type 2 diabetes patient with impaired islet function.
In just 11 weeks the patient was no longer dependent on external insulin!
33 months later this potentially transformative study has been published in the Journal of Cell Discovery. For that entire duration, the 59-year-old male patient has been insulin free!
The team at Shanghai Changzheng Hospital with the Shanghai Institute of Biochemistry and Cell Biology, Center for Excellence in Molecular Cell Science have showcased a truly revolutionary new therapy that could change the way that we manage and treat type 2 diabetes.
Here’s what you need to know.
First off... what is type 2 diabetes
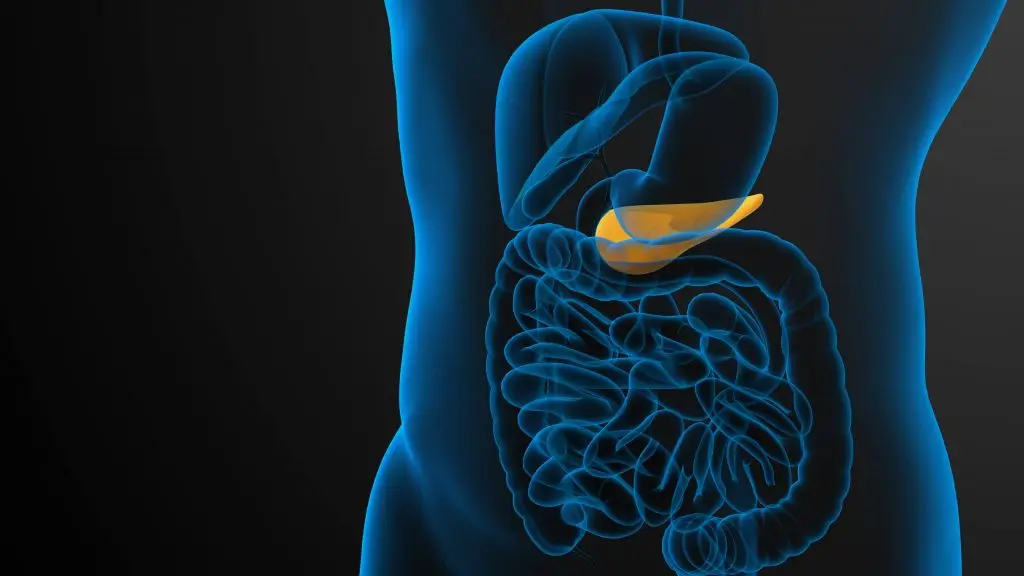
Type 2 diabetes is a chronic condition characterised by insulin resistance and a gradual loss of endogenous insulin production as islet cells in the pancreas overwork to produce insulin and manage blood glucose levels. Once a patient has been diagnosed with type 2 diabetes, they have already lost 50 – 70% of their insulin-producing cells, and as a result, one-third to half of type 2 diabetes patients ultimately require exogenous insulin.
Emerging advancements
Recent treatments such as islet transplantation have seen some success in type 1&2 diabetes, but are limited by the shortage of donor organs, prompting the need for alternative therapies.
Recent research has shown that pancreatic progenitor cells or islet tissues derived from human pluripotent stem cells (hPSCs) can survive, function, and reverse hyperglycemia in diabetic models. However, these are just models and the approaches are complicated by the risk of tumor formation and the presence of undifferentiated cells.
This solution
The researchers experimented with personalised stem cells derived from the patient’s own cells, which created insulin-producing islet cells genetically identical to the patient. This method eliminates the risk of immune rejection and avoids the limitations in sourcing donor organs.
The result
The patient, who had been dependent on insulin injections for years, became insulin-independent in just 11 weeks post-transplantation. Over the next 33 months, the patient remained free from insulin therapy, showcasing the potential of this treatment to provide a long-term cure for type 2 diabetes.
Future implications
Is this approach going to revolutionise current treatments for type 2 diabetes?
The answer is not clear-cut.
Personalised medicine, especially using stem cells is extremely promising and may be the primary treatment option for type 2 diabetes and other diseases in the future. By creating therapies that are uniquely tailored to an individual’s genetic profile, the treatment’s efficacy is greatly enhanced. It also avoids adverse events such as immune rejection, which is a significant hurdle in current transplantation therapies. As current treatments for type 2 diabetes don’t offer a permanent cure, this treatment approach will likely steer us on the path to discovering a robust and permanent cure.
China also has a disproportionately high prevalence of diabetes amongst the population and holds the highest number of people with diabetes globally. As a result, this breakthrough is highly significant, as any advancement in finding a lasting cure for type 2 diabetes will impact millions of people.
Limitations
Unfortunately, this treatment has only been effective in the one patient and has not gone through the clinical trial process – a vital component of the drug discovery pipeline. This approach would need to be repeated successfully in much more substantial research to even be considered as a broad cure for type 2 diabetes.
Another major limitation of this technology is its scalability. Producing personalised islet cells for potentially millions of diabetes patients, calls for some significant advancements in our biomanufacturing processes.
Currently, the cost of stem cell therapies can be astronomically high which results in a vast barrier to accessibility. Research such as this contributes to lowering this barrier and promotes further investigation into this treatment option in the future.
Despite these limitations, the use of stem cell-derived islet cells in a lasting type 2 diabetes cure for this patient, represents a significant breakthrough in diabetes treatment overall. Continued research, innovations, and breakthroughs will be vital in the future to translate this exciting approach into a practical therapy for the millions of diabetes patients globally.